
 |
 |
rev. 04-03-00
This information is provided as an informational forum with
permission from the source; Ralph Fergis, Life Science Department, Palomar
Community College, San Marcos, CA.
THIS INFORMATION CANNOT BE USED
WITHOUT PERMISSION UNLESS IT IS USED FOR A CLASS ASSIGNMENT OR NON PROFIT USE.
Regardless, please give credit to the web author and web site and
Ralph Fergis
So, I hope the following information is helpful...
The heart begins showing rhythmic contractile activity very early in embrological life (between 15 and 21 days after fertilization) and continues this activity until death. It is a very effecient pump. But at this early age the heart is not yet an effective pumping organ. Within sereral days after vascular tissue formaton, the fluid precursor to blood flow is occuring. This is the beginning of blood flow, the vascular system, and the cardiac pump.
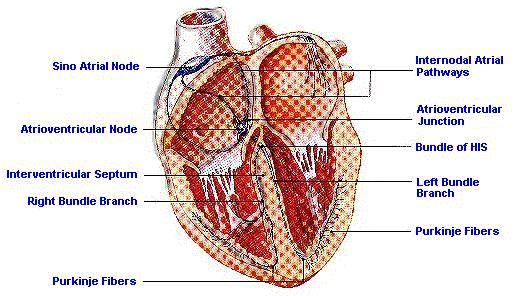
In order for the heart to be an effective pumping organ, it must be able to maintain this cyclic fashion and be able to maintain this for as many as 80 to 100 years. The system responsible for this repeated contraction cycle is compossed of the Sino-Atrial Node (SA), the Inter-Nodal Pathways, the Atrio-Ventriacular Node (AV), the Common Bundle (of HIS), the Right and Left Bundle Branches, and the associated Purkinjie Fibers. These structors contribute to form an intrinsec system of excitation and electrical conduction that produces and maintains the hearts cyclic contractile activity.
The sinoatrial node and the atrioventicular node both exhibit rhythmic electrical activity. These nodes and the purkingie fibers that make up the conduction system are all embriological, made from cardiac muscle. However, these cells have become specialize for electrical activity rather than contractility. Remember that both muscle and neurons have action potentials associated with their cell membranes, therefore this specialization represents a modification in function, rather than a new function. Because of this specialization, these cells conduct impulses faster than the other caridac cells.
These cells, as well as other cardiac cells also have cyclic depolarizations that lead to action potentials. The cardiac cells are linked electrically through the intercolated disc. Those cells whose cycle depolarizations occur at the fastest rate control the frequency of all other cells. The sinoatrial node has the highest intrensic frequency and therefore dominates the frequency of contraction. In its absence the atrioventricular node or the other structors control the system.
The SA Node is located in the right atrial wall near the opening for the Superior Vena Cava. From this position in the heart it releases cyclic depolarizations. Moving through the Atria via cell to cell conduction. This depolarization spreads from near the point of stimulation to adjacent areas. Following this spread of the depolarization through time, it appaers similar to a wave on a still pond that is the rsult of a single small pebble. The wave moves from the point of impact and spreads in all directions equally. This depolarization moves through the atria in a similar fashion. Because the atrial muscle mass is made up of cells of a variety of types and organizational patterns the depolarization wave will move through the atria a little faster in some areas than others. The further the distance traveled by the action potential the longer the time period required to reach the destination.
Due to the large build up of connective tissue that supports the valve structures at the junction of the atria and ventricals this wave of depolarization is effectively prevented from entering the ventricular musculature by conduction through the adjoining muscle mass. This prevents the spread of the SA Node generated action potential from stimulating the superior protion of the ventricaular mass. In this mannner the ventricles are prevented from contracting from the top down and instead are stimulated to contract from the appex (bottom) up. After the AV node is stimulated and sends the impulse down through the Bundle of His. The AV Node is located at the base of the the right atrium near the junction of the four heart chambers.
Connecting the SA and AV nodes are internodal pathways. These "pathways" are a series of purkinjie fibers that take a more direct route between these nodes than the rest of the cardiac cells in the Atrium. It appears that, although these fibers are not a distinct anatomical structure, they do not exist isolated from each other. They do preform an important physiological function. They conduct the depolarization of the SA Node to the AV Node faster than the wave of depolarization as it progresses between these structures through the atrial muscle mass. In this manner the AV Node is assured of receiving the depolarization at a constant time in the cycle rather than relying upon waiting for the depolarization wave to move through the atrial muscle mass.
If the signal is channeled back through the Nodal Pathway by an abnormality (extra fibers) or due to other physiological events, the heart rate is increased and most likely doubled or trippled. This is called an SVT or Supra Ventricular Tackycardia.
As the signal leaves the AV Node it is sent to the Common Bundle, which is also named the Atrioventricular Bundle or the Bundle of His. This bundle of purkinjie fibers leaves the AV Node and progresses down the interventricular septum towards the apex (bottom) of the heart. After a short distance, the bundle splits into right and left branches that eventually spreads to the leaft and right ventricular cardiac musculature of the heart and to the apex of the heart. Once the bundle branches reach the apex of the heart the individual purkinjie fibers branch out to the ventricular myocardium. There are a great number of fibers in the left bundle branch and this branch is functually slightly faster and stronger than the right branch. This combined with a larger muscle mass, the left ventricle produces a more powerful contraction.
Now, consider the timing function of these structures. This discussion will be based upon a normal heat beating at a resting rate of 72 per minute with each cycle requiring about 0.8 seconds to complete. After this concept is understood, the individual anatomical structures will become more clear.
Perform the mathematical conversion:
72 beats per minute = 0.8 sconds per heart beat.
You will now
understand where the 0.8 seconds came from.
|
|
= |
|
Now consider a typical clock. When we learned about clocks in about the first grade several ideas and concepts were established. Our clock system is based upon 60 seconds per minute, 60 minutes per hour and 24 hours per day. Therefore manufacturers build clocks according to the standards of the day. What if instaed we based our clock on 100 seconds per minute, 50 minutes per hour and 20 hours per day. If this is what we considered normal, then manufacturers would build a clock to this new set of standards.
Now build a "cardiac clock." It will look similar to the clock on the wall. This clock will start at the top like the one we use to tell time. The numbers will get larger around the the outside as time progresses. And, as the hands progress clockwise from the top, to the right side, to the bottom, to the leftside they will get back to the top. At that point in time the numbers change just like a real clock counting the seconds, hours or days.
There are several diferences between the cardiac clock and a typical clock. The cardiac clock has only a "second" hand. If typical clocks had only second hands, then we could only count seconds and they would be called a minute clock. They would cycle each and every minute. Without the other hands a clock is useless to tell other aspects of time. A typical 60 second clock has 60 time divisions and starts with zero at the top, 15 at the right, 30 at the bottom, 45 at the left, and 60 at the top. However, once 60 is reached in a typical clock, we start counting again and start at zero for the begining of the next clock cycle. The 0.8 second clock will have only eight divisions with 0 at the top. 0.2 at the right, 0.4 at the bottom, 0.6 at the left, and also implied, as well as shown is 0.8 at the top. The "cardiac clock" meets the same exact criteria set down for typical clocks but is based upon a different time cycle. Rather than 60 seconds or one minute per cycle, this clock is based upon 0.8 seconds which represents the time for one cardiac contraction cycle at 72 beats per minute..
Each cardiac cycle starts with the depolarization released from the SA Node. Once this depolarization is released it is picked up by the internodal pathways and travels rapidly to the AV Node. The atrial muscle mass begins to contract. This wave of depolarization spreads through the atrial musculature causing them to contract beginning closest to the original point of stimulation. Just as there is a wave of depolarization moving through the Atria, there is also a wave of contraction. Immediatly behind the wave of contraction is repolarization and then relaxation. Those myocardial cells which receive the depolarization early will conduct early and will also relax early.
In this way, four types of waves move through the Atria and the Ventricles.
They are:
It takes about 0.1 seconds for the wave of contraction to move throughout the Atria. It also takes about 0.1 seconds for a wave of relaxation to move through the Atria. From the clock above, it is clear that the Atria contracts for 0.1 seconds and relaxes for 0.1 seconds. The Atria rests for 0.6 seconds. Consider that both relaxation and rest are both passive events, it is easy to see that the Atria works for 0.1 second and rests for 0.7 seconds in an 0.8 second clock.
At the time that the Atria complete their contraction the Ventricles begin to contract. The AV Node will release the depolarization which originated from the SA Node into the Bundle of HIS and the Right & Left Branches and to the Myocardium at the apex of the heart. The interventricular myocardium begins contracting at essentially the same time that the Atria finish which is at 0.1 second on the clock. The apical ventricular muscle mass begins to contract about 0.05 - 0.07 seconds later. The wave of depolarization spreads through the ventriacles progressing from the apex towards the top of the chambers. There is a very minor amount of depolarization that progresses into the ventricles from the atria because of the large mass of connective tissue at the atrioventricular junction. These chambers are effectively electrically isolated.
As the apical depolariaztion progresses there is contraction and then relaxation flowing into the ventricles. Because of the large muscle mass of the ventricles, the portion nearest the apex begins and completes contraction beforte other areas. On the clock, the ventricular contraction takes about 0.3 seconds for complete contraction. Also you will see that relaxation takes about 0.3 seconds and begins about 0.1 second after ventricular contraction. The portion of the heart which contracts first relaxes first and there is considerable overlap in time durring this process. The lower portion of the ventricles begin to relax while the upper portion is still contracting. Total ventricular relaxation is complete by about 0.5 seconds and the ventricles completely rest for about 0.4 seconds or untill 0.1 seconds of the next cycle.
The time values presented here are not absolutely perfect. They are however close enough for the purpose of understanding cardiac timing. For the common man, the values given for contraction time hold very near to constant at all heart rates. If the heart rate changes to a slower or faster rate, the contraction and timing durations do not change. So if a heart is beating at 180 beats per minute there would be minimal time for rest and the ventricles will not be 100% full when they contract.
|
|
= |
|
In this case the atria contracts at the same rate of 0.1 second and relaxes for 0.1 second. The atria will only have 0.1 second to rest. The ventricles contract for 0.3 seconds and relaxes somehwhat simultaneously as it overlaps but has only 0.1 second for rest. The ventricles have very little time for free flow filling, so cardiac output is deminished. It is easy to see that someone in an Supra Ventricular Tackycardia (SVT) will have a difficult time compensating and providing adequate blood flow. In a worse case senario Ventricular Tackycardia, the atria is not contracting as it is being over riden. In a Thrid Degree Block there is no sequence between the atria and the ventricles so the ventricles cannot fill appropriately prior to contraction.
Makes sense???
If you have any further question, please send E-mail. If this information is used for a class paper or project, please provide the appropriate references.
Thank you...
By, Mitch Mendler E.M.T. paramedic / firefighter,
 to S.D. Medic 12 lead for
more information...
to S.D. Medic 12 lead for
more information...
Genentec Inc.More information and educational Software from these companies:

Click here to send E-Mail to
The San Diego Medic Association.
To contact Eric Yeargain send him E-Mail here.
Click here to go back to the main page: The San Diego Paramedics

Web page design and maintenance by Mitch Mendler E.M.T. Paramedic;The WebMaster!
 The Beginning |
 Navigation |
S.D. Dispatch |
S.D. Paramedics |
S.D. MedNews On-Line |
E.K.G. |
 LINKS |
Public Safety |
 Maltese Cross |
 Saint Florian |
 Fire Dogs and Horses |
 The Magic Wand |